
PGS and PGD IVF is a combination of procedures that apply the latest scientific breakthroughs in order to evaluate the genetics of an embryo before placing the embryo in the womb. We have been performing PGS and PGD IVF since June of 2000. Our first live birth was reported in 2001. Since then, FC & AG of Florida has been at the forefront of PGD/PGS in the Southeastern United States.
We are happy to announce the continuation of our progress with another first for Florida and the Southeastern United States. We are happy to report our first pregnancies with 24 chromosome microarray technology in October of 2009 and our first pregnancies in 2012 after laser assisted trophectoderm blastocyst biopsies using complete genomic hybridization technology. Fertility Center and Applied Genetics of Florida and Dr. Pabon have one of the broadest experiences in Pre-implantation Genetics in the Southeastern United States.
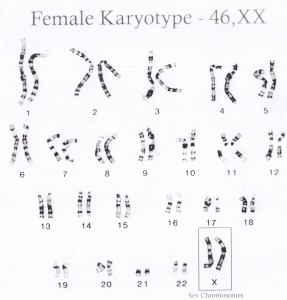
The cells of our bodies have genetic information that is mostly in the nucleus of the cell. In the nucleus there are 23 pairs of chromosomes that carry the genetic information given to us by our genetic mother and father. We receive one of each pair from our mother’s egg and our father’s sperm.
The information in the DNA molecule condensed into the chromosomes in each of our cells. One important function of our gonads is to duplicate and separate the chromosomes as eggs and sperm are made. Unfortunately, the duplication process is far from perfect and produces eggs and sperm with an abnormal number of chromosomes quite often.
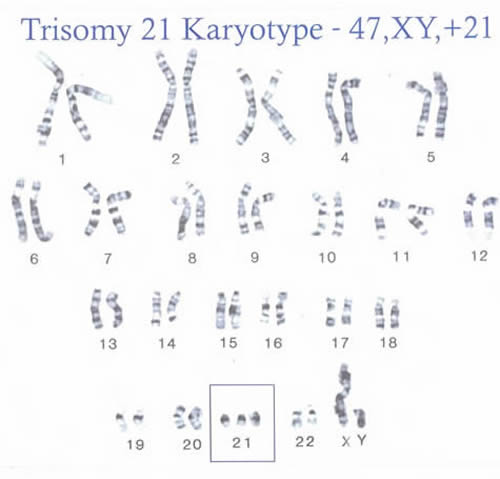
Think of the gonads as a copying machine that must copy 3,000 million DNA letters and then collate them into chromosome data books. This has to be done thousands of times in the ovary and many billions of times in the testicle. Errors that occur in nature usually result in a failed conception, a miscarriage, or an abnormal child with an extra chromosome like in Down’s syndrome. With IVF and PGD technology we can find many mistakes before the embryo is implanted.
In order to perform PGD, patients must undergo “in vitro” fertilization. Eggs are harvested and subsequently fertilized. PGD requires insemination of single eggs with single sperm in order to avoid having multiple sperm cells from being adherent to the outer shell of the egg after standard insemination procedures. The fertilization of a single egg with a single sperm cell is achieved with the intracytoplasmic sperm injection procedure (ICSI).
This is an insemination technique that has been practiced since the early 1990’s very routinely for severe male factor infertility. ICSI is required for PGD in order to be certain that genetic test results are those of the embryo and not those of a single sperm cell that happened to be picked up as part of the embryo biopsy.

The embryo biopsy required for PGD can be performed on multicellular day 3 embryos or blastocysts. After fertilization, the fertilized egg divides into 2-4 cells the next day. The following day (day 3 post fertilization) the embryo is usually made up of 6-10 cells. A small opening is made in the outer sugar coating (zona pellucida) of the embryo with either an acid solution or a laser.
Then one or two cells is aspirated or teased out, collected, packaged, and sent to the reference laboratory for testing.

Day 3 biopsies are still performed in special situations. Day 3 biopsies have been largely replaced by day 5 and 6 blastocyst trophectoderm biopsies. This is due to the higher reliability of the results when the trophectoderm is tested as compared to only one or two cells from a day 3 embryo.
Copyright photo from Julio E. Pabon, M.D. collection
In the above photo the inner cell mass is the group of cells between one and three o’clock. The trophectoderm cells are all the smaller surrounding cells best seen from six to nine o’clock. Sperm cells are visibly attached to the zona pellucia at seven and nine o’clock. Therefore, this blastocyst was the result of a non-ICSI “standard” insemination procedure six days earlier.
The trophectoderm of the embryo is the part of the embryo that is destined to become the placenta. The genetic testing of the trophectoderm cells matches the genetics of the part of the embryo (the inner cell mass) that becomes the fetus and subsequently the baby with a higher accuracy than the biopsies on the third day of embryo growth. It is estimated that the genetic evaluation of the trophectoderm agrees with the inner cell mass with greater than 98% accuracy.
That being said, patients must understand that there can be no absolute guarantee of 100% accuracy in medicine and genetics. The trophectoderm biopsy of a day 5 or 6 blastocyst begins with the laser assisted hatching of the outer sugar coating (the zona pellucida). This small opening is usually made with the microscopic laser on the third or fourth day of culture. The embryo is replaced in the incubator and two days later they checked for signs of herniation of the trophectoderm. When the trophectoderm is “peeking” out, the microscopic laser is used to dissect a few cells. These cells are packaged and sent to the reference laboratory for the desired genetic test.


The cells obtained are processed by our reference laboratories. In the first years of the PGD program, these cells were processed for analysis using fluorescent in situ hybridization techniques FISH. We and many other laboratories have gradually moved to complete genomic hybridization techniques that evaluate all 24 human chromosomes. Patients must understand that even the latest complete genomic hybridization techniques are not infallible. Limitations of the technology include and may not be limited to the following:
The cells obtained may not yield a “reading” or result.
The cells sampled cannot be assumed to represent the genetics of the baby 100% of the time.
Even a “normal” reading does not guarantee a “normal” baby.
A “normal” reading should be interpreted as “normal within the limits of the test” and the fact that only a few cells were tested and not the whole embryo.
If a patient is scheduled for day 5 or 6 blastocyst biopsies, the biopsies can only be performed if the patient’s embryos reach the blastocyst stage. There may be some patients that do not have any blastocysts for biopsy. Similarly, those that plan day 3 biopsies may not have any embryos reach the required 5 or more cells for biopsy.
Patients that plan a fresh embryo transfer may only have available for transfer those normal embryos that are biopsied on the third or fifth day. Embryos that reach the blastocyst stage on the sixth day will have to be frozen.
Patients that choose the “all freeze” protocol must understand that there can be no absolute guarantee of the survival or recovery of frozen embryos.
There is a very rare risk of damage to an embryo during these procedures.
Not all genetic defects are detectable using this technology of PGD.
Testing for single gene mutations involves different technology that is not ordered or performed unless it has been determined that the patient has a very high risk (25-50%) of conceiving a baby with one of these diseases. Standard PGD focuses on confirming that the embryo most likely has two pairs of each of the 23 chromosomes.
Standard PGD counts chromosomes in the smallest unit of life, one cell. The test does not examine tiny micro-events that occur along the inside of the DNA of these chromosomes. That type of testing is many times more expensive and is usually reserved for a different field of medicine (pediatrics or peri-natology).
Even though these processes are very accurate, there is no absolute 100% guarantee of either a normal child or the gender of that child.
Signing this document gives Dr. Pabon, the embryologists, and/or designated assistants permission to discard genetically abnormal embryos.
The above described procedures are optional and have been recommended in order to try to improve our chances of achieving a normal pregnancy with IVF.
PGD that screens for chromosome number problems (aneuploidy) in embryos or specialized screening for a specific disease in an embryo does not eliminate the need for routine pregnancy screening with prenatal tests like chorionic villus sampling, amniocentesis, or some of the newer maternal blood screens that can screen fetal cells in maternal circulation for genetic abnormalities.
Chromosomes are structures found in the center or nucleus of cells. A human has 46 chromosomes (23 pairs). Each of us received 23 chromosomes from our mother and 23 chromosomes from our father. Chromosomes are made of very long strands of DNA. Regions of the DNA strands in chromosomes are organized into definite coding regions called genes. Particular genes contain the code for particular protein molecules that direct or carry out all the millions of functions of our bodies.
Having an extra portion of a chromosome or a missing portion of a chromosome is called aneuploidy. This can result in failure of implantation of the embryo, pregnancy loss, and other conditions such as infertility and congenital abnormalities such as Down’s syndrome (Down’s syndrome results when the embryo and subsequent child has extra genetic information in the form of an extra chromosome 21.
Mosaic embryos are less of a problem with Blastocyst BiopsiesCurrently, most clinics still perform embryo biopsies on the third day of embryo culture by sampling one or two cells from an embryo composed of 5 to 10 cells. Multicellular embryos can be made of different cell types. Most research has shown that any single embryo has about a 7%-10% chance of being mosaic. This means that if we sample a cell, that cell may not represent the part of the embryo that will become the fetus and baby.
This means that the results are not absolute or “guaranteed”. Nothing is absolute or guaranteed in medicine and genetics. After performing hundreds of day 3 biopsies since 2001, our clinic has never had an error regarding a diagnosis as it applies to a baby’s PGD/PGS. Nonetheless, more and more research and information has emerged over the years about the lower risk of false or incorrect results from trophectoderm blastocyst biopsies as compared to the multicellular day 3 embryo biopsies.
For that reason, our clinic’s PGD/PGD program has moved to the biopsy of the trophectoderm of blastocyst as the primary technique for PGD/PGS. Even a trophectoderm biopsy cannot guarantee that the results are 100% correct all the time.
It is estimated that the results of PGD/PGS with complete genomic hybridization to determine if an embryo has 23 pairs of chromosomes is more than 98% accurate. The accuracy of the Pre-implantation diagnosis of single gene diseases is unique to each probe and or disease being tested for. Due to the possible mosaicism in embryos and the limits of the technology, we always advise our patients to have all the standard obstetrical testing without regard for what was tested prior to the pregnancy.
Genetically abnormal (aneuploid) embryos can be indistinguishable in appearance and development from chromosomally normal ones. The PGD/PGS results can guide the selection of embryos for replacement into the mother. Most chromosomally abnormal embryos either do not implant or spontaneously abort shortly after implantation. Thus, if only normal embryos are replaced, each embryo will have a higher chance of implanting and reaching term.
The probability of conceiving a healthy child is increased through PGD/PGS. PGD/PGS for aneuploidy has been reported to increase implantation rates in several studies, to reduce the rate of pregnancy loss by half and to increase take-home baby rates.
The benefits of PGD/PGS increase when more embryos are available for analysis. If there are fewer than six embryos, there may not be any increase in the pregnancy rate. Nonetheless, even with few embryos, the information gained from PGD/PGS can assist in the decisions involved in an IVF cycle.Patients with specific chromosomal rearrangements (like translocations) or specific gene or DNA defects can avoid passing this to their offspring through the application of PGD/PGS. The list of known single-gene defects for which we have specific probes grows each week.
Visit our website for a list of some of the conditions that can be tested for with PGD/PGS.
Performing embryo biopsies is not without risk of injury to the embryo. Thus far, we estimate the risk of damage to any biopsied embryo as less than one percent. Embryos that have been biopsied in our laboratory have developmental rates comparable to age-matched and diagnosis-matched controls.
That is, the biopsy process does not appear to hurt embryos in our laboratory. Nonetheless, patients must realize that the PGD/PGS process involves a micromanipulation that could injure a dividing embryo so that it may subsequently arrest or degenerate.
Even with microarrays, there is no guarantee that results will be available on all the embryos or all the chromosomes. Microarray technology does not give results regarding every single gene in an embryo. Early embryonic development is complex. It has been shown that human embryos can develop into an abnormal or disorganized fetus even in the presence of a completely normal complement of 23 pairs of chromosomes.
Most of the time, these abnormal pregnancies abort spontaneously. Patients must understand that PGD/PGS may fail in individual cases because of unforeseen technical malfunctions. It is not possible to guarantee pregnancy after PGD/PGS or even promise that there will be benefits for any individual case. Additionally, there are rare diseases where the genetic problem lies in places other than the DNA in the chromosomes in the nucleus of the cell. These are the inherited mitochondrial inherited diseases for which PGD/PGS technology is not yet available.

Your Next Step:
Get your consultation time
by clicking the button below
or by calling 941-342-1568.