Sex selection with IVF by Laser blastocyst trophectoderm biopsies and PGS with microarray 24 chromosome complete genomic hybridization techniques in our Florida Clinic is the most accurate method available.
While most clinics that provide Sex selection with IVF services are still depending on older technology based on the biopsy of a day 3 embryo and FISH (Fluorescent in situ hybridization probes), we have been pioneers in the application of blastocyst biopsies in the Southeastern United States. The technology is so reliable that the majority of treatments can be completed with a single embryo transfer (fresh or frozen/thawed) with an expectation of pregnancy in more than 75% of patients that receive a single embryo after a fresh embryo transfer.
Remarkably, in 2013, patients that were treated with “all freeze” protocols for the transfer of a single tested (euploid) blastocyst achieved a pregnancy in more than 90% of cases when embryos were implanted into a normal uterine lining.
We have been offering PGD, PGS, and Sex selection with IVF services since 1999. Our first pregnancy with PGS/PGD technology and Sex selection with IVF was in a treatment completed in late 1999. At that time and until mid 2012, all of our procedures were based on day 3 embryo biopsies. Recently, we have brought the capability of blastocyst biopsies to the Southeastern United States.
Emerging science continues to confirm the safety and increased reliability of the results based on the biopsy of the blastocyst. The results for PGD, PGS and Sex selection with IVF are so reliable that we have increased our pregnancy rates while reducing the number of embryos transferred from 2 or 3 to only one in most cases. This allows completion of the treatment without the risk of a complicated multiple (twin or triplet) pregnancy.
Technology has advanced significantly in the past several years allowing couples the option of selecting the sex of their next child. Fertility Center & Applied Genetics of Florida and the offices of Julio E. Pabon, M.D., P.A. participated in the MicroSort® clinical trial. Dr. Pabon had a long association with the MicroSort® study team as a study collaborator.
The microsort trial had hoped to reliably sort sperm in order to reliably select a sample rich in Y chromosomes (to lead to a male child) or rich in X chromosomes (to lead to a female child), but the trial failed. There were never reliable enough results to bring it to clinical fruition. Research continues in this area of science. Unfortunately, thus far sperm sorting procedures are not reliable enough for clinical use. At this time the only reliable method for family balancing or sex selection requires “in vitro” fertilization and pre-implantation genetic diagnosis or screening of pre-embryos prior to implantation.
Pre implantation Genetic Screening (PGS) or Pre implantation Genetic Diagnosis (PGD) for Sex Selection with IVF (family balancing)
PGS stands for pre-implantation genetic screening of embryos. PGD stands for pre-implantation genetic diagnosis of embryos. PGS or screening is the term for the procedures involved in determining that an embryo or embryos have the correct or incorrect number of chromosomes. PGD or genetic diagnosis of embryos is the term for the procedures (very similar in the IVF lab) that lead to diagnosing a particular disease or condition in the embryo that has to do with a particular genetic disease.
PGD is usually performed to test embryos when the parents are “carriers” of a particular disease like Cystic fibrosis, spinal muscular atrophy, Fragile X, sickle cell anemia, etc. For the purposes of screening embryos in order to determine their gender, PGD is carried out to determine the number of chromosomes and which sex chromosomes are present. PGS also helps to prevent conditions that are caused by genetic errors in the numbers of chromosomes in embryos like the Down’s syndrome (trisomy 21) or other conditions like it where the embryo may have an incorrect number of chromosomes and may be used as part of sex selection with IVF.
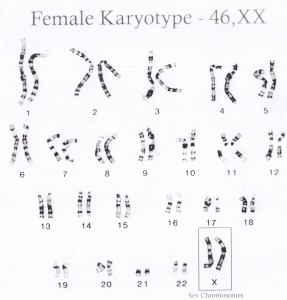
Humans with a normal complement of chromosomes have 23 pairs of chromosomes. There are 22 pairs of chromosomes called the autosomes that determine characteristics other than gender. In addition to these 22 chromosomes, there is a pair of “sex chromosomes” that carry the genetic information that leads to the differentiation of the fetus into a girl or a boy. The Karyotype of a girl is 46 XX while that of a male is 46 XY. The presence of the Y chromosome leads to differentiation into a boy. The figure below is a computer enhanced image of the chromosomes in the nucleus of cell.
The sex of a pre-embryo can be determined three, five, or six days after the fertilization of the egg. Our center had its first live birth after PGD/PGS sex selection IVF in 2000. The patient carried a sex-chromosome-linked fatal genetic disease. In this initial case, we were able to screen three day old pre-embryos for abnormalities in eight key chromosome pairs. One of the chromosome pairs was the sex chromosomes. We were able to select XX carrying female pre-embryos to transfer into the mother. This avoided the severe neurological disease that was carried in the male offspring in this family. Since then, we have treated numerous patients with PGD or PGS for not only sub-fertility, recurrent pregnancy losses, genetic disorders, as well as patients with a desire to pre-determine the sex of the next child.
Our patients are always counseled that no medical procedure can be 100% guaranteed. It should be noted however that since 2002, we have treated hundreds of patients without one misdiagnosis or surprise regarding the sex of the child.
PGD/PGS technology has become more reliable. In the first years of PGD/PGS, we relied mostly on the biopsy of day 3 multicellular pre-embryos. Day 3 multicellular pre-embryos are usually composed of 6-8 cells. While most pre-embryos are made up of identical cells, 7-10% of them can be mosaics. Mosaic multicellular pre-embryos can lead to a sampling error that can give erroneous results since the cell sampled may not represent what ultimately becomes the baby. In addition, in the early years of this technology, we relied mostly on fluorescent “in situ” hybridization techniques in order to identify the chromosomes. The probes used for “in situ” hybridization were designed to bind to unique regions of chromosomes and relied on binding affinities that varied with each assay. Nonetheless, we were able to have very reliable results with not a single misdiagnosis even in the early years.
Since 2006, our program evolved to more reliable 24 chromosome microarrays and complete genomic hybridization techniques. These complex technologies expand the available DNA in a cell and give a reading of the genetics of the cell that is more reliable than the old “FISH” techniques. Even more recently, as of the Fall of 2012, our program has moved from day 3 multicellular pre-embryo biopsies to the highest current technology. This is the laser assisted trophectoderm blastocyst biopsy.
Laser assisted trophectoderm blastocyst biopsies raise the bar to the highest possible level because we sample embryos on the fifth or sixth day and we sample more than one cell per pre-embryo. This increases the reliability and reduces the negative impact of mosaicism. One can be 98%-99% sure that the results of the embryo biopsy will represent the ultimate genetics of the fetus and subsequent baby. Please refer to the PGD/PGS portion of this web page.
At Fertility Center & Applied Genetics of Florida and the offices of Julio E. Pabon, M.D.,P.A., we treat all pre-embryos with great respect and encourage families to preserve through cryopreservation normal pre-embryos regardless of their sex chromosome status.
The ethics of sex selection are certainly controversial. There are certainly those who feel that this technology should only be applied to prevent devastating genetic diseases or conditions. Some feel it should not be an elective procedure used for family balancing. Family Balancing & Sex Selection is an extremely personal decision. We are fortunate to have the freedom to make such choices. Choosing one blastocyst pre-embryo over another certainly is better than choosing further along in the fetal stages of the pregnancy.
Given the safety of the processes involved, it is our opinion that family balancing through sex selection is acceptable. The processes are carried out on pre-embryos prior to any tissue differentiation or organ system development. Blastocyst pre-embryos have not yet developed any differentiated tissues such as nerve tissues or cardiac tissues. The potential for development exists just as in the stem cells in the bone marrow, the dermis of the skin, and even in the menstrual cells shed each month.
Patients must understand that there may not be any normal pre-embryos in any particular treatment cycle. Very abnormal pre-embryos may arrest or stop growing prior to reaching the blastocyst stage for biopsy. Also, the results of the genetic tests may not yield a normal chromosome complement of the desired gender. These results are very disappointing, but are a reality of the biology involved. Patients must decide whether they wish to freeze normal pre-embryos of the opposite sex desired or if they would accept them for implantation. Alternatively, the embryos can be placed in an adoption program managed by our offices. A treatment may be a scientific success while still being disappointing.
Patients will have a thorough consultation that can be in person (local patients) or via SKYPE or on the phone. Dr. Pabon prefers SKYPE instead of the phone because he can share his desktop with the patients and show tables and images to patients during the remote consultation. Patients will be prepared for IVF in the usual manner. They will be required to do some routine labs and pre-tests as described in the IVF patient guide. Out of town patients can be prepared by their local physicians or clinics and travel to Sarasota at the very end of the ovarian stimulation phase.
Modern IVF procedures are extremely safe. There have been recent changes in the ovarian stimulation and the egg maturation trigger that have virtually eliminated the risk of severe ovarian swelling or “ovarian hyperstimulation syndrome.” In years past, the final trigger was with full dose hCG. This led to ovarian hyperstimulation in 10-25% of patients depending on their clinic protocols. Severe hyperstimulation was the most feared complication as it could lead to hospitalization and even severe complications like blood clots. Recently, we have applied new science in order to trigger most of our higher responding patients with a very gentle “agonist trigger.” This strategy leads to a very mild ovulation that leads to only mild ovarian enlargement and exceeding low risks of ovarian hyperstimulation. The only down side is that the agonist trigger results in lower implantation rates and therefore these cycles lead to the harvest of the eggs and the IVF and embryo biopsies, but the blastocysts have to be frozen for implantation the following month.
The other common complication that is feared by most specialists is a twin or higher order pregnancy. Fortunately, this complication is quite rare now that we are able to complete most treatments with a single embryo transfer.
Dr. Pabon advices against the transfer of more than one “robust” embryo with normal genetic results. In years past and in patients being treated without PGS testing of their embryos, it was quite common to implant 2 embryos. The reason for this is that one cannot tell if an embryo is genetically normal based on its appearance. Implanting 2 embryos without PGS results in average pregnancy rates of 45-50% in good prognosis patients in their early and mid thirties. Implanting one “robust” embryo with known normal PGS genetic results results in a pregnancy in more that 60% of patients. Implanting 2 in this situation has resulted in 100% twins in every case robust embryos were transferred (at the time of this writing). A planned twin pregnancy is not good medicine because these pregnancies are very risky for the babies due to pre-term birth and much higher chances of severe congenital anomalies and cerebral palsy.
Our Medical and Laboratory Director:
Julio E. Pabon, M.D. , F.A.C.O.G.

Your Next Step:
Get your consultation time
by clicking the button below
or by calling 941-342-1568.