Risk of ovarian cancer is not associated with ART in long-term cohort study
This is very reassuring information for our patients. This was shared from the premier European journal called Human Reproduction
Published 6 days ago
A study which cross-linked more than 30,000 Dutch ART patients to the national cancer registry with follow-up over a mean of 24 years found they had a greater risk of ovarian cancer than women in the general population but no greater risk than in an untreated group of sub-fertile women.
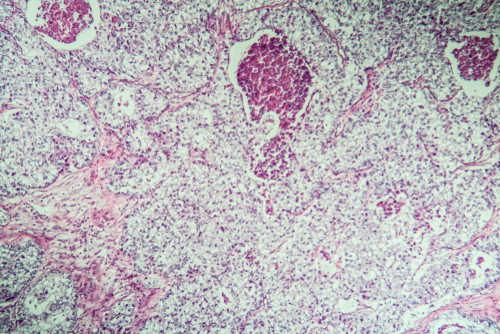
The first large-scale cohort study to assess the long-term association of ovarian cancer with ART has found that women treated with IVF and ICSI are at no greater risk than untreated infertile women.(1) A greater risk of ovarian cancer found in treated subjects than in the general population was attributed to the higher prevalence of nulliparity in the ART-treated women.
The study, whose preliminary results were presented at ESHRE’s 2019 annual meeting in Vienna, was based on a cohort of more than 30,000 sub-fertile women who received ovarian stimulation for ART between 1983 and 2000 in the Netherlands and were cross-linked to the national cancer registry and Dutch Pathology Registry until 2018. Median follow-up was 24 years. The risk of ovarian tumours in the ART-treated women was compared with risks both in the general population and in almost 10,000 sub-fertile women not given ART. This was, said the authors, the first study able to examine whether unsuccessful ART cycles carry a different risk of ovarian tumours from successful cycles.
Results showed ovarian cancer risk in the ART group was significantly higher than in the general population (standardised incidence ratio 1.43, 95% CI 1.18-1.71) but was still comparable with the non-ART group. The investigators thus concluded that the increased risk of ovarian cancer in the ART group (as also found in the non-ART sub-fertile group) ‘appears to be’ explained by ‘nulliparity rather than ART treatment or specific subfertility causes’. It was also found that ART-treated women with more successful cycles had a statistically significantly reduced risk of ovarian cancer, whereas a larger number of unsuccessful cycles made no difference to the risk estimates – again, emphasising the adverse effect of nulliparity on ovarian cancer risk.
The authors note that the risk of ovarian cancer from ART has long been a biologically explicable cause for concern, increasing in its public health implications with the advancing use of ART. They note that many epidemiological studies have investigated the association with ovarian tumours but with inconsistent results. In 2013, for example, two meta-analyses were published showing that women who received fertility treatments were more likely to develop ovarian cancer than women in the general population.(2,3) Despite the concerns, however, and the increasing data, results have remained inconclusive.
It was also found that women in this study who received ART appeared to have an almost two-fold higher risk of borderline ovarian tumours, both when compared with the general population and with infertile women not receiving treatment. However, these risks did not increase after additional treatment cycles or after longer follow-up. This lack of ‘dose response’, said the authors, suggested that the higher risks for borderline tumours might be because of underlying patient characteristics rather than the treatment itself. They noted that borderline tumours are ‘rare in the general population and are generally easy to treat’.
In a press release issued by the journal publisher, the study’s lead author, Flora van Leeuwen from the Netherlands Cancer Institute, said that ‘reassuringly, women who received ovarian stimulation for assisted reproductive technology do not have an increased risk of malignant ovarian cancer, not even in the long run’. She did warn, however, that the median age of the women at the end of study follow-up was only 56 years, and the incidence of ovarian cancer increases with age.
Meanwhile, an exhaustive meta-analysis of cohort or case-control studies has found that endometriosis was associated with 1.9-fold greater risk of ovarian cancer than in women without endometriosis in 24 eligible studies.(4) However, as with nearly all evidence in all cancers the study data displayed high heterogeneity, and most were subject to bias. Indeed, the authors name ‘the strong evidence for publication bias’ as ‘a warning for journal editors’, suggesting that any association between endometriosis and ovarian cancer could be an overestimate. ‘This may be driven by a belief by reviewers and editors that any study that does not demonstrate this positive association is incorrect,’ they add, ‘but it may also reflect that as ovarian cancer is very rare extremely large cohort sample sizes or multi-site case-control studies are needed to yield power to quantify statistical significance .’
The meta-analysis also quantified positive associations between endometriosis and breast (4% greater risk) and thyroid cancers, but found no association with endometrial cancer.
The authors rightly ask in their conclusions what the results mean for women with endometriosis and the doctors who treat them. Their answer lies first in a recognition of the likelihood of bias in studies so far, and next in the conversion of relative to absolute risk. Thus, they explain, ‘updating this absolute estimate [1.8%] with the quantified risk estimate from the present meta-analysis [standardised RR 1.93], this absolute risk increased to 2.5%, which is 1.2% higher than the absolute risk for women without endometriosis and still very low’.
Nevertheless, the authors note that their results raise several public health implications, particularly the apparent lack of association with endometrial cancer and a protective association with cervical cancer. However, they conclude, ‘given their low absolute risk of ovarian, breast and thyroid cancers and the uncertainty with regards to their risk of other cancer types, general prevention messages may be delivered to patients with endometriosis: to be aware of well-demonstrated cancer risk factors and to focus on aspects of wellness demonstrated to reduce cancer risk’.
1. Spaan M, van den Belt-Dusebout AW, Lambalk CB, et al. Long-term risk of ovarian cancer and borderline tumors after assisted reproductive technology. J Natl Cancer Inst 2020; doi:10.1093/jnci/djaa163.
2. Li L, Zhou J, QianX J, et al. Meta-analysis on the possible association between in vitro fertilization and cancer risk. Int J Gynecol Cancer 2013; 23: 16–24.
3. Siristatidis C, Sergentanis TN, Kanavidis P, et al. Controlled ovarian hyperstimulation for IVF: impact on ovarian, endometrial and cervical cancer – a systematic review and meta-analysis. Hum Reprod Update 2013; 19: 105–123.
4. Kvaskoff M, Mahammat-Saleh Y, Farland LV, et al. Endometriosis and cancer: a systematic review and meta-analysis. Hum Reprod Update 2020; doi:10.1093/humupd/dmaa045

