New Recommendations for Older Infertility Patients
As a Florida IVF Doctor or Reproductive Endocrinologist, I agree with the new recommendations for older infertility patients. In our Florida IVF clinic in Sarasota and Bonita Springs, I have been discussing the new recommendations for older IVF patients for quite some time. Richard Reindollar’s team has reported in both the “Fast-track” study and in the “Fort T” studies that patients should made aware of the differential chances of pregnancy associated with different treatments. He has demonstrated that older patients benefit from more aggressive treatment like IVF sooner rather than later.
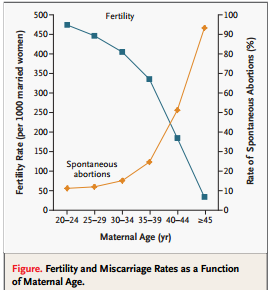
As I discuss on a daily basis, older patients have a decreased chance of pregnancy because they make more genetically abnormal embryos. In the past, many good Ob/Gyns and Reproductive Endocrinologists were hesitant about moving patients quickly to IVF due to the fear of multiple pregnancies and associated severe complications like pre-term birth and a much higher risk of neonatal morbidity, mortality, and congenital anomalies associated with twin and higher order pregnancies. With current scientific advances, even older patients can be treated with single embryo transfers after pre-implantation genetic screening of blastocysts. The application of PGS for a planned single “Euploid” (and embryo with 23 pairs of chromosomes) transfer allows patients of all ages to have implantation rates with a single embryo that are higher that even implanting 3 or more embryos that have unknown genetic makeup.
Below is a recent Bulletin from the American Society of Reproductive Medicine detailing the results of these studies:
ASRM Bulletin
Volume 16, Number 25
May 6, 2014
Highlights from Fertility and Sterility
Older Women Should Move More Quickly to IVF
A new study demonstrates that, for couples of older reproductive age with unexplained infertility, immediate IVF is the most efficient treatment, resulting in fewer treatment cycles and a higher live birth rate.
In an NIH-funded, randomized clinical trial, 154 couples receiving infertility treatment at Boston IVF and Brigham and Women’s Hospital were randomly assigned to one of three groups to receive a specific type of treatment for their first two cycles. One group was assigned to have IVF. The other two groups were assigned to have intrauterine inseminations (IUI) with the female partner receiving either an oral medication to induce ovulation (clomiphene citrate- CC) or injectable ovulation drugs (follicle stimulating hormone-FSH).
If patients in the two insemination groups did not achieve an on-going pregnancy after two cycles, they were switched to IVF for their subsequent cycles.
The participating couples were required to have been trying to conceive for at least six months and to not have previously tried any of the treatments being used in the study. The female partner had to be between 38 and 42 years old, with regular menstrual cycles, at least one ovary and fallopian tube, acceptable ovarian reserve, no disorders of the reproductive organs and no history of ectopic pregnancy. The male partner had to have enough motile sperm.
After two cycles of the assigned treatment, differences were observed in pregnancy rates and live births between the groups. Of patients who went straight to IVF, 49% became pregnant and 31% gave birth. Of those taking oral medications and having inseminations, 22% became pregnant and 16% gave birth. For the injectable medication/insemination group, 17% became pregnant and 14% gave birth.
All couples who had not been successful in their first two cycles of any treatment used IVF in their subsequent treatment cycles, but the couples in the immediate IVF group of the study went through 36% fewer total cycles than the couples who began their treatment in either of the ovulation drug/IUI groups.
By the end of the treatment, of all the couples in the study, 71% had conceived a clinical pregnancy and 46% delivered at least one live-born baby. 84% of all live births in the study came about as a result of IVF. For those couples having a live birth, those who started with IVF took an average of two cycles to conceive, while those who started with ovulation drugs and IUI averaged three to four cycles. Of the 154 couples enrolled, 140 started and 115 completed treatment.
While the major finding of this study is that immediately starting infertility treatment with IVF in older couples is the most effective treatment, it also showed that, if a couple chooses to try ovulation drugs with insemination first, oral fertility drugs (clomiphene citrate) are as effective as injectables (FSH).
Richard Reindollar, MD, Executive Director of the American Society for Reproductive medicine (ASRM) was the study’s principal investigator when he was at Dartmouth Hitchcock Medical Center (DHMC), prior to ASRM. He described how the study came about. “Previously, in the Fast Track and Standard Treatment (FAST-T) trial, we found that for young couples with unexplained infertility, proceeding to IVF after three cycles of clomiphene with IUI was more cost-effective than the standard approach at the time- which required them to go through several additional cycles of injectable ovulation drugs with insemination before allowing them to try IVF. We suspected that immediate IVF without any prior cycles with IUI would be more effective in an older age group but needed to demonstrate that through a rigorous trial.” Marlene Goldman, ScD, Professor at DHMC and first author of the paper stated, “While we recognize that not all patients might choose to start treatment with IVF, the results of this trial will give reproductively older patients with unexplained infertility the evidence they need to skip less effective treatments and start their families more quickly if they wish to do so.”
Goldman et al, A randomized clinical trial to determine optimal infertility treatment in older couples: the Forty and Over Treatment Trial (FORT-T), Fertility and Sterility, in press.


