Basic Infertility information.
Approximately 15% of couples experience infertility or subfertility. Infertility or subfertility is defined as the inability to conceive and deliver a child after one year of trying. The definition has been expanded recently to include patients that have been trying to conceive for six months and are older than 38 years of age. This recent change was brought about in order to encourage patients and physicians to begin an evaluation earlier in the older group. The main reason to begin the evaluation earlier in older patients is that these patients are in a time of their lives when their reproductive ability is decreasing rapidly mainly due to genetic issues. Please review the maternal age and reproduction part of this web site as well as the Pre-implantation Genetics page.
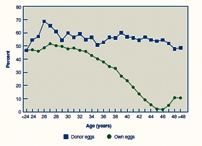
Fecundity is defined as the percentage probability that a couple will conceive a pregnancy in a given month. (Insert reference here). The monthly fecundity rates are very much related to the age of the female partner. Fecundity decreases with age. See maternal age and reproduction document. Very clear information regarding this issue can be gained by looking at the following two graphs. Graph A shows the decrease in pregnancy rates with age as well as the likelihood of infertility as related to age. Graph B shows that the pregnancy rates are not affected by the age of the woman when a donor egg is used.
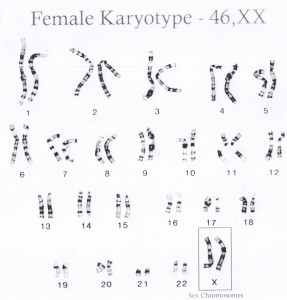
Older patients are known to have a higher chance of numerical chromosomal abnormalities in their children. Numerical chromosomal problems arise from “nondisjunction” problems as chromosomes segregate as the oocyte (egg) is maturing in preparation to be fertilized. Human oocytes are formed early in the embryonic development of the female fetus. It is estimated that each female fetus and then child is born with about 250,000 eggs. These eggs are in the outer surface of the ovary and are genetically “arrested” in an intermediate part of the first cell division called prophase 1 of Meiosis 1. The object of meiosis cellular divisions of the gamete or oocyte is to reduce the number of chromosomes in half so that the usual cell that has all the information to make a human and contains 23 pairs of chromosomes end up making cells that contain one half the information; that is, 23 single chromosomes. The problem is that the chromosomes are very large molecules that carry our DNA information. They are so large that if all the chromosomes from a single human cell were uncoiled and unravelled, the strand of DNA could reach the moon!! Not only are chromosomes large molecules, they are electrically charged and quite sticky. After resting all “bunched up” in the nucleus of the human egg for many years and in a space more than 1,000 times smaller than the “dot” at the end of this sentence, segments of chromosomes and even entire chromosomes can “go the wrong way”. The end result is the generation of an egg that has an abnormal number of chromosomes. The two images below show examples of a normal chromosome panel of a woman and an abnormal chromosome panel as found in a child with “Down’s syndrome” or trisomy 21 (three copies of chromosome 21).
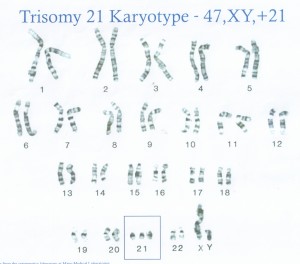
This error in Meiosis is called nondisjunction. It can result in an infinite number of aberrant chromosome complements in fetuses. Fortunately, most pregnancies with aberrant chromosome complements result in a miscarriage. The most common cause of miscarriages is the 45XO karyotype where a conceptus is missing a sex chromosome. Other commonly seen abnormalities include trisomy 15 and trisomy 21. Herein lies the limit of reproduction as we know it. Chromosomal abnormalities in eggs and subsequently the embryo and fetus are the main reason why pregnancy rates decrease with maternal age while miscarriage rates increase with maternal age. The table below is a table that relates the age of the mother at the time of delivery with the risk or chance of discovering a chromosomal abnormality in the fetus with standard obstetrical screening (amniocentesis).
Risk of Down’s Syndrome and Chromosomal Abnormalities at Live Birth, According to Maternal Age
| Maternal Age at Birth | Risk of Down’s Syndrome   | Risk of a Chromosome Problem |
|---|---|---|
| 20 | 1/1667 | 1/526 |
| 25 | 1/1200 | 1/476 |
| 30 | 1/952 | 1/385 |
| 35 | 1/378 | 1/192 |
| 40 | 1/106 | 1/66 |
| 45 | 1/30 | 1/21 |
Data for table modified from Hook et al from Chromosomal Abnormality rates at amniocentesis and Live born Infants. JAMA 1983; 249:2034-8
One may note, for example, that at the age of 30, the risk that down’s syndrome is 1 in almost 1000 while the risk at 40 years of age is ten times higher (approx. one in one hundred). The news is not all bad. A 41 year old patient has a 2% chance of having a child with a chromosomal problem. A significant part of the problem is that many embryos and even fetuses are lost very early in development due to severe abnormalities that are incompatible with life. Many times these early losses don’t make it past the fourth or fifth week of pregnancy. Sometimes these embryos don’t even make it to implantation.
Experience with pre-implantation genetic diagnosis (PGD or PGS) has given results that are consistent with previous clinical experience. Pre-implantation genetic diagnosis is described in those sections of this web site. In short, we are able to know the genetic makeup of embryos before they are implanted in the womb. The trend over the years has been that younger patients have more normal embryos while older patients have mostly genetically abnormal embryos. Abnormal embryos cannot be implanted.
Male factor problems are another common cause of infertility or subfertility. Infertility in couples can be attributed to a male factor problem in about 35% of the time. Simply put, the lower the number of normal, motile sperm in the ejaculate, the lower the chance of pregnancy. There are genetic causes, structural causes, toxic exposure causes, as well as hormonal causes of low sperm counts. An extensive discussion of the subject can be found in the semen analysis document and in Dr. Pabon’s IVF guide.
Tubal Factor and Peritoneal Factor Subfertilty / Infertility
The fallopian tubes are responsible for carrying the sperm to the ampullary part of the fallopian tubes where the egg is usually fertilized. After fertilization, the pre-embryo or embryo travels down the fallopian tube into the uterus where the embryo implants and develops into a fetus. Tubal factor infertility is a common cause of infertility or subfertility. Patients may have tubal scarring from old bacterial infections like gonorrhea or chlamydia. Scarring may also be the result of chronic processes like endometriosis. Endometriosis is the finding of endometrial tissues that have attached in parts of the body outside of the womb. This “ectopic” endometrial tissue can continue to cycle with the menstrual cycles of the patient and lead to inflammatory processes that can lead to scarring of the tubes and other parts of the pelvis. Endometriosis may be suspected if a patient has significant menstrual pain as well as subfertility. Endometriosis can be diagnosed with ultrasound if very typical findings are seen within the ovary. The ultrasound is usually described as revealing endometriosis cysts in the ovaries (endometriomas) that have a typical appearance of dense homogenous echoes consistent with a blood filled cyst. If discovered, these cysts need to be followed up because they can be confused with normal post ovulatory “corpus luteum” cysts. Most commonly, the only way to diagnose endometriosis is with surgical procedure called a laparoscopy. Not all patients need to have a laparoscopy. If the clinician suspects significant endometriosis and the patient’s only symptom is subfertility or infertility, then there is really no need to do a laparoscopy. In the past, clinicians used to think that it was beneficial to “clean up” the endometriosis. Unfortunately, this led to much unneeded surgeries. Patients had extensive laser laparoscopies and surgical treatment for multiple small endometriomas only to end up being treated with IVF anyway. Recent randomized treatment studies have shown that patients do better avoiding extensive surgeries for “asymptomatic” endometriosis and going straight to IVF.
Endometriosis is an enigmatic condition. It is present in 15% of women in the general population, but may be present in as many as 35% of infertility patients with normal partners. Oftentimes patients found to have minimal endometriosis may have the most pain symptoms like painful periods or painful intercourse. The treatment of symptomatic patients usually requires a laparoscopic diagnosis, followed by chronic suppression therapies with oral contraceptives, progesterones, and even androgens. Some patients may be so refractory that they may need to be put into a temporary menopause with the use of Lupron or Depot Lupron. Depot Lupron therapy is usually just temporary as the endometriosis and the symptoms return after it is stopped. Depot Lupron will lead to low estrogen levels and has the risk of leading to bone loss. Fortunately bone loss in young women is often reversible. There is no need to place a young woman on Depot Lupron after surgical treatment as it only delays childbearing with no real benefit in boosting pregnancy rates.
The usual infertility evaluation begins with a history and physical exam, some prenatal labs, pre-conception genetic screening for cystic fibrosis, spinal muscular atrophy, fragile X as well as other recessive conditions. Then a semen analysis is performed. Once the semen analysis is found to be normal, Dr. Pabon may order a hysterosalpingogram or HSG. The HSG is an x ray procedure where the physician will instill a contrast solution through the cervix and into the uterus and tubes. The HSG test gives a lot of information about the patient’s anatomy. If the HSG is very abnormal, Dr. Pabon may recommend further evaluation with an ultrasound or even a diagnostic laparoscopy.

The HSG is not an uncomfortable procedure when done well. Dr. Pabon has been performing his own HSGs since 1990. He uses a technique that does not require having to pass catheters into the womb. Most patients take a tylenol or 600 to 800mg of ibuprofen one hour prior to the HSG and report no significant discomfort.
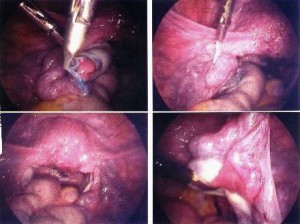
Who needs a laparoscopy is a difficult question. Some patients may have abnormalities on the physical exam or the HSG that lead to a high suspicion of endometriosis or scar tissue. Some patients may simply wish to have a complete infertility evaluation prior to continuing to try to conceive. More and more patients are foregoing the laparoscopy and moving through to a trial of artificial inseminations or even to IVF. If the patient is a good candidate for a laparoscopy, Dr. Pabon will perform it in the most minimally invasive way and probably use the CO2 laser during the procedure to vaporize endometriosis or dissect adhesions. Tubal factor problems are the cause of infertility in about 40% of the patients. Nowadays it is more common for tubal factor infertility patients to forego the surgical interventions and move on to IVF. Nonetheless, patients are presented with all the choices.
The Uterine factor
The physical exam, the HSG and/or an ultrasound can discover abnormalities of the uterus or womb. Commonly found problems include uterine fibroids or myomas and uterine anomalies like a uterine septum.
Uterine Fibroids
Uterine fibroids or myomas are quite common. By the age of 40, more than 50% of patients have at least a small insignificant myoma. Fibroids are best described as benign (non-cancerous) growths of the muscle wall of the uterus. They can appear in the inside of the uterus (intracavitary), in between the cavity and the lining (submucous), in the muscle wall (intramural), on the surface of the uterus (subserosal), or outside the uterus with a small connection (pedunculated).
Fibroids may present with obvious symptoms like abnormal uterine bleeding, pain, or pressure. Some patients may have a history of subfertility or a miscarriage. The HSG and the ultrasound can help to determine the location and number of fibroids. Most importantly, Dr. Pabon will determine whether a particular fibroid presents a problem. Problem fibroids can be removed from within the uterus with a hysteroscopic technique that requires no incisions. Sometimes, Dr. Pabon recommends temporary shrinkage of the fibroid prior to removal in order to diminish the surgical risks and facilitate the procedure. Some uterine fibroids require either a laparoscopy or a traditional myomectomy or removal with an incision. Recently there has been some advances pertaining to robotic assisted surgeries. Unfortunately, the robotic surgery often results in a less cosmetic result than a mini-incision due to the numerous small incisions required for this type of surgery. Fortunately most significant fibroids can be removed without an incision or with a very small low bikini incision.
Dr. Pabon and many reproductive surgeons will commonly use medical therapies in order to temporarily shrink uterine myomas prior to surgery. Depot Lupron has been used for this for many years. It is an injectable monthly medication that can induce a temporary menopause. With low estrogen levels, the uterine myomas will usually reduce in size by 50% or more and allow their removal with a minimally invasive procedure and with lower risk of bleeding since the myoma’s blood supply also reduces after 2-6 months of Depot Lupron treament.

Ovarian dysfunction and the Polycystic Ovary Syndrome
gynecology clinic, but may be referred to a Reproductive Endocrinology practice like Dr. Pabon’s when initial evaluation and treatment fails to yield results.
Patients with ovulatory problems or dysfunction can present with irregular or absent menstruation, short menstrual cycles, prolonged menstrual cycles, and even with failed urine luteinizing hormone assays (the over the counter ovulation predictor kits).
When assessing a patient with such history, Dr. Pabon evaluates patients for the many causes of these problems such as thyroid problems, pituitary problems, hypothalamic problems, insulin resistance and hyperandrogen states. That is why he recommends ordering a laboratory panel that includes ovarian and pituitary hormones. There is really no need to check adrenal hormones like DHEAS because their over-production usually is detected with an elevated total testosterone level.
The TSH level.
This is Thyroid Stimulating Hormone. It is a hormone produced by the pituitary gland to stimulate the thyroid gland to make thyroid hormone. The TSH level is low when thyroid hormones are oversecreted and TSH is high when there is a low level of thyroid hormone. Low thyroid or hypothyroidism is very common. As many as 50% of women develop this during their lifetimes. Often this is the result of an autoimmune condition that results in the eventual loss of thyroid hormone secretion. When the pituitary senses a low level of thyroid hormone it secretes more TSH. The TSH can cross react with other parts of the pituitary gland and lead to an increase in prolactin. Too much prolactin can inhibit ovulation and lower estrogen levels. All this is resolved with a thyroid hormone supplement
The prolactin level
As mentioned above, high prolactin levels may be a secondary response to a low thyroid hormone level. Another common cause of a moderately elevated prolactin level is a benign pituitary tumor called a microadenoma. Microadenomas are quite common. When an elevated prolactin level is discovered in the presence of normal thyroid hormone studies, then an MRI of the brain is indicated. If a pituitary tumor is discovered to be smaller than one centimeter, then it is called a microadenoma. Larger tumors require further evaluation with neurologists and neurosurgeons for follow up and treatment. Fortunately most tumors are small and don’t require surgery. They can be treated with dopamine agonist medications like Bromocriptine (parlodel) and Dostinex. These medications usually lead to a lowering of the prolactin level and even fibrosis of the adenoma and correction of the problem. Normal ovulation usually returns when the prolactin levels normalize.
The Follicle Stimulating Hormone and Luteinizing Hormone levels
These two hormones are secreted by the anterior pituitary and their secretion in a regular pattern is required for the ovarian follicles to respond with the recruitment, maturation, and eventual ovulation of the lead oocyte. The level of these hormones and their pattern give the Reproductive Endocrinologist insight into what may be the cause of the ovulatory problem. If the level of these hormones is very high, then the patient may be facing premature menopause. If the level of these hormones is very low, then the patient may have dysfunction of the hypothalamus signals to the pituitary. This hypothalamic dysfunction may be due to starvation, physical, or mental stress. Avid exercisers can reduce the FSH and LH levels to the point that they don’t ovulate, have periods, or even have such low estrogen levels that they develop early osteopenia or osteoporosis.
The pattern of the FSH and LH hormones may give a hint of other conditions like polycystic ovaries. These patients often have an LH level that is higher than the FSH level.
The polycystic ovary syndrome can be best explained by the main symptom which is ovarian dysfunction or anovulation. These patients have very irregular or infrequent menstruations. Some never menstruate without medication (a progesterone challenge). The syndrome of the polycystic ovary includes anovulation, irregular periods, increased male hormones and androgen effects, and usually a polycystic appearance of the ovary on ultrasound. Please note that many young patients have many small antral follicles on ultrasound that can mimic a PCO appearance. Most PCO patients are overweight. In many the increased weight leads to insulin resistance. Insulin resistance is believed to be central to the pathophysiology of PCO syndrome. In obese PCO patients, insulin levels are higher than normal. The higher insulin levels can lead to ovarian dysfuction due to aberration in the maturation process of oocytes. This aberration is associated with an increase in the secretion of ovarian male hormones. It is unclear what comes first, the elevation in the ovarian androgens or the hypersecretion of the LH hormone. Elevated LH hormone levels stimulate the ovarian tissues to secrete more male hormone and also stimulate the adrenal gland to do the same. Interestingly, Dr. Pabon was the lead investigator in discovering the presence of LH/hCG receptor in the human adrenal gland during his fellowship in Reproductive Endocrinology and Infertility at the University of Louisville.
The treatment of the PCO patient may be as simple as a low carbohydrate diet for weight loss. This is the quickest and best way to decrease weight, decrease the insulin resistance and eventually ovulate. PCO patients that become more fit have an easier time ovulating when ovulation drugs are used. Some patients still require insulin sensitizers like Metformin or even Clomid. Some very refractory patients may need to use injectable FSH in the minimal stimulation protocol. This minimal stimulation FSH protocol is highly successful in inducing ovulation in the most difficult patients. Dr. Pabon will discuss all options with patients and even review surgical induction of ovulation with the “ovarian drilling” procedure if needed. This surgical approach is effective but more rarely used due to worries about the risk of the formation of peri-ovarian adhesions.
Infertility/Subfertility treatments…a current update
In summary, when you consult with a Reproductive Endocrinologist regarding infertility or subfertility, you should expect a thorough evaluation that is efficient and cost effective. After enough information is gathered, you will be presented with options for further evaluation or treatment. If all the tests are normal, you will be presented with strategies to try to improve your chance of pregnancy. Very important considerations for this are the age of the patient and the length of time that they have been trying to conceive.
If specific problems are identified, then the possible solutions to these problems will be discussed and may include hormonal treatments or surgeries. As a board certified Reproductive Endocrinologist and Infertility specialist, Dr. Pabon has all the training and experience necessary to address gynecological hormonal and surgical problems regarding infertility and its causes.
A heart warming story about Infertility:
“Christine and Ryan began talking about children in October 2009, and the couple married Feb. 6, 2010. Christine had her first consultation with Lakewood Ranch Medical Center’s Dr. Julio Pabon in April 2010. After two failed intrauterine inseminations, the couple opted for an in-vitro fertilization treatment in November 2010.
“We got a Gia bean,” Christine says, smiling at her newborn.
Ryan, who will care for Giavanna once Christine starts back to work in a few weeks, already is getting proficient at changing diapers, feeding the baby and handling other day-to-day newborn-related tasks from his wheelchair. ” Full Story Here

Your Next Step:
Get your consultation time
by clicking the button below
or by calling 941-342-1568.
